7.1 Finding Rational Solutions of Polynomial Equations a B Answers
Overview and Statistics
What are the case definitions for reportable HBV infections?
Case definitions have been developed by CDC, in collaboration with the Council of State and Territorial Epidemiologists, to provide uniform clinical and laboratory-testing criteria for the identification and reporting of nationally notifiable infectious diseases. The case definitions for acute, chronic, and perinatal hepatitis B are available at the following links:
- Acute hepatitis B
- Chronic hepatitis B
- Perinatal hepatitis B (Acquired in the United States or U.S. Territories)
How many new HBV infections occur annually in the United States?
In 2018, a total of 3,322 cases of acute hepatitis B were reported to CDC, for an overall incidence rate of 1.0 cases per 100,000 population (1). After adjusting for under-ascertainment and under-reporting, an estimated 21,600 acute hepatitis B cases occurred in 2018 (1).
Has the rate of new HBV infections in the United States changed?
The rate of reported acute hepatitis B cases has remained stable over the past decade, with a slight increase occurring in 2017 (1).
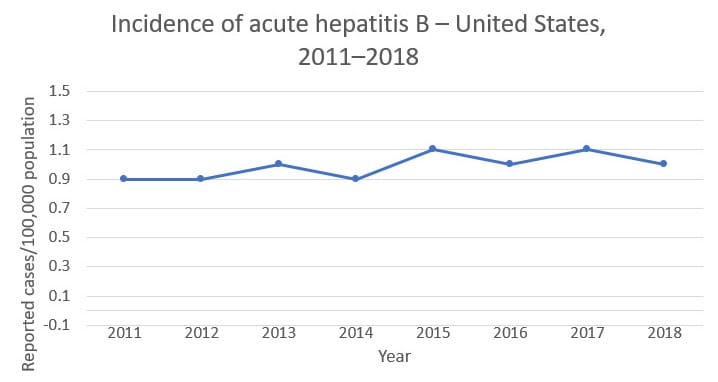
Source: CDC, National Notifiable Diseases Surveillance System.
How common is chronic HBV infection in the United States?
In 2016, an estimated 862,000 people were living with HBV infection (3).
How many deaths can be attributed to chronic HBV infection?
In 2018, a total of 1,649 U.S. death certificates had HBV recorded as an underlying or contributing cause of death (7). However, this is a conservative estimate.
Transmission, Symptoms, and Treatment
How is HBV transmitted?
HBV is transmitted through activities that involve percutaneous (i.e., puncture through the skin) or mucosal contact with infectious blood or body fluids (e.g., semen and saliva), including
- sex with an infected partner;
- injection-drug use that involves sharing needles, syringes, or drug-preparation equipment;
- birth to an infected mother;
- contact with blood from or open sores on an infected person;
- exposures to needle sticks or sharp instruments; and
- sharing certain items with an infected person that can break the skin or mucous membranes (e.g., razors, toothbrushes, and glucose monitoring equipment), potentially resulting in exposure to blood.
How long does HBV survive outside the body?
HBV can survive outside the body and remains infectious for at least 7 days (2).
What should be used to clean environmental surfaces potentially contaminated with HBV?
Any blood spills (including dried blood, which can still be infectious) should be disinfected using a 1:10 dilution of one part household bleach to 10 parts of water. Gloves should be worn when cleaning up any blood spills.
Who is at risk for HBV infection?
The following populations are at increased risk for becoming infected with HBV:
- Infants born to infected mothers
- Sex partners of infected people
- Men who have sex with men
- People who inject drugs
- Household contacts or sexual partners of known people with chronic HBV infection
- Health-care and public-safety workers at risk for occupational exposure to blood or blood-contaminated body fluids
- Hemodialysis patients
Who should be screened for HBV?
CDC recommends that the following people be screened for HBV (3,4,5):
- People born in countries with an HBV prevalence of ≥2%
- People born in the United States not vaccinated as infants whose parents were born in regions with high rates of HBV infection (HBsAg prevalence of ≥8%)
- Men who have sex with men
- People who inject drugs
- People with HIV
- Household and sexual contacts of HBV-infected people
- People requiring immunosuppressive therapy
- People with end-stage renal disease (including hemodialysis patients)
- Blood and tissue donors
- People with elevated alanine aminotransferase levels (>19 IU/L for women and >30 IU/L for men)
- Pregnant women (hepatitis B surface antigen [HBsAg] only is recommended)
- Infants born to HBV-infected mothers (HBsAg and antibody to hepatitis B surface antigen [anti-HBs] only are recommended)
Are international travelers at risk for HBV infection?
The risk for HBV infection in international travelers is generally low, except for certain travelers to regions where the prevalence of chronic HBV infection is high or intermediate (i.e., HBsAg prevalence of ≥2%). Hepatitis B vaccination should be administered to unvaccinated people traveling to those countries. More information about hepatitis B and travel is available from CDC's Travelers' Health site.
What are the signs and symptoms of HBV infection?
Not all people with acute HBV infection have symptoms. The presence of signs and symptoms varies by age. Most children <5 years of age and newly infected immunosuppressed adults are generally asymptomatic, whereas 30%–50% of people age ≥5 years have signs and symptoms (6). When present, signs and symptoms of acute HBV infections can include
- fever,
- fatigue,
- loss of appetite,
- nausea,
- vomiting,
- abdominal pain,
- dark urine,
- clay-colored stool,
- joint pain, and
- jaundice.
Most people with chronic HBV infection are asymptomatic and have no evidence of liver disease or injury. However, some people develop chronic hepatitis (elevation of AST/ALT), cirrhosis, or hepatocellular carcinoma (i.e., primary liver cancer).
What is the incubation period for hepatitis B?
If symptoms occur, they begin an average of 90 days (range: 60–150 days) after exposure to HBV (7,8).
When symptoms of acute hepatitis B occur, how long do they usually last?
Symptoms typically last for several weeks but can persist for up to 6 months (7,8).
How serious is acute HBV infection?
Acute infection ranges from asymptomatic or mild disease to fulminant hepatitis, although the latter occurs only rarely. Disease is more severe among adults age >60 years (1).
How serious is chronic HBV infection?
Approximately 25% of people who become chronically infected during childhood and 15% of those who become chronically infected after childhood die prematurely from cirrhosis or liver cancer, and most remain asymptomatic until onset of cirrhosis or end-stage liver disease (9,10).
How likely is HBV infection to become chronic?
The risk for chronic infection varies according to the age at infection and is greatest among young children. Approximately 90% of infants and 25%–50% of children aged 1–5 years will remain chronically infected with HBV. By contrast, approximately 95% of adults recover completely from HBV infection and do not become chronically infected (6).
What tests are used to identify patients with hepatitis B?
Three different serologic tests are needed (hepatitis B surface antigen [HBsAg], hepatitis B surface antibody [anti-HBs], and total hepatitis B core antibody [anti-HBc]) to determine whether a patient
- has acute or chronic HBV infection and is in need of post-test counseling and linkage to care (11),
- is immune to HBV as a result of prior infection or vaccination (in conjunction with vaccination history), or
- is susceptible to infection and in need of vaccination.
For detailed information about HBV screening and specific serologic markers, see Interpretation of Hepatitis B Serologic Test Resultspdf icon .
How long after exposure to HBV can HBsAg be detected in an infected patient's blood?
HBsAg will be detected in an infected person's blood an average of 4 weeks (range: 1–9 weeks) after exposure to the virus. About half of patients will no longer be infectious by 7 weeks after onset of symptoms, and all patients who do not remain chronically infected will be HBsAg-negative by 15 weeks after onset of symptoms (8).
Where can I learn more about HBV serology?
CDC offers an online training that covers hepatitis B serology.
How is HBV infection treated?
People with acute infection are provided supportive treatment depending on their symptoms. For people with chronic infection, several antiviral medications are available (12); these patients require linkage to care with regular monitoring to prevent liver damage and/or hepatocellular carcinoma. The American Association for the Study of Liver Diseases (AASLD) has published practice guidelines for the treatment of chronic hepatitis Bexternal icon.
What is HBV reactivation?
HBV reactivation is the abrupt reappearance or rise in HBV DNA in a patient with previously inactive chronic or resolved hepatitis B. It is often accompanied by a flare in disease activity with elevation of liver enzymes with or without symptoms. HBV reactivation can be severe, resulting in death (13).
Who is at greatest risk for HBV reactivation?
Patients who test positive for both anti-HBc and HBsAg are at substantially higher risk of reactivation than are those who are positive for both anti-HBc and anti-HBs. Others at risk include people
- undergoing cancer chemotherapy;
- taking immunosuppressive therapy, including
- Rituximab and other drugs that target B lymphocytes (black box warning),
- high-dose steroids, and
- anti-TNF agent;
- with HIV infection who have discontinued therapy with antiretroviral drugs that also have activity against HBV;
- undergoing solid organ or bone marrow transplantation; and
- being treated for HCV coinfection.
For more information on risk, monitoring, and prevention of HBV reactivation, see the American Gastroenterological Association's Institute Guideline on the Prevention and Treatment of Hepatitis B Virus Reactivation During Immunosuppressive Drug Therapyexternal icon and AGA Institute Guidelines on Hepatitis B Reactivation (HBVr): Clinical Decision Support Toolexternal icon.
Are patients undergoing treatment for HCV at risk for HBV reactivation?
Because of recent reports of HBV reactivation in HCV coinfected patients receiving direct acting antiviral (DAA) therapy for HCV (14), all patients initiating HCV DAA therapy should be tested for HBV with HBsAg, anti-HBs, and anti-HBc. People testing positive for HBsAg and/or anti-HBc should be monitored while receiving HCV treatment. More information about treating HBV/HCV coinfected patients can be found at http://hcvguidelines.orgexternal icon and https://www.aasld.org/publications/practice-guidelines-0external icon.
What is HBV/hepatitis D virus (HDV) superinfection?
Superinfection occurs when people with chronic, active HBV infection are subsequently infected with HDV. Superinfection exacerbates the symptoms of the chronic HBV infection and can lead to acute liver failure (see Hepatitis D FAQs for Professionals).
Hepatitis B Vaccination
Who should be vaccinated against hepatitis B?
The Advisory Committee on Immunization Practices (ACIP) recommends that the following people receive hepatitis B vaccination:
- All infants
- Unvaccinated children aged <19 years
- People at risk for infection by sexual exposure
- Sex partners of people testing positive for hepatitis B surface antigen (HBsAg)
- Sexually active people who are not in a long-term, mutually monogamous relationship (e.g., people with more than one sex partner during the previous 6 months)
- People seeking evaluation or treatment for a sexually transmitted infection
- Men who have sex with men
- People at risk for infection by percutaneous or mucosal exposure to blood
- People who currently inject or have recently injected drugs
- Household contacts of people who are HBsAg-positive
- Residents and staff of facilities for developmentally disabled people
- Health care and public safety personnel with reasonably anticipated risk for exposure to blood or blood-contaminated body fluids
- Hemodialysis patients and predialysis, peritoneal dialysis, and home dialysis patients
- People with diabetes aged 19–59 years; people with diabetes aged ≥60 years at the discretion of the treating clinician
- International travelers to countries with high or intermediate levels of endemic hepatitis B virus (HBV) infection (HBsAg prevalence of ≥2%)
- People with hepatitis C virus infection
- People with chronic liver disease (including, but not limited to, people with cirrhosis, fatty liver disease, alcoholic liver disease, autoimmune hepatitis, and an alanine aminotransferase [ALT] or aspartate aminotransferase [AST] level greater than twice the upper limit of normal)
- People with HIV infection
- People who are incarcerated
- All other people seeking protection from HBV infection
Is hepatitis B vaccination recommended in certain settings?
Yes. In certain health-care, evaluation, or treatment settings, a high proportion of clients have known risk factors for HBV infection. ACIP recommends universal vaccination of adults who receive care in those settings, which include:
- sexually transmitted disease treatment facilities,
- HIV testing and treatment facilities,
- facilities providing drug-abuse treatment and prevention services,
- health-care settings targeting services to people who inject drugs,
- correctional facilities,
- health care settings targeting services to men who have sex with men,
- chronic hemodialysis facilities and end-stage renal disease programs, and
institutions and nonresidential day care facilities for people with developmental disabilities.
What are the hepatitis B vaccines licensed for use in the United States?
Three single-antigen vaccines and two combination vaccines are currently licensed in the United States.
Single-antigen hepatitis B vaccines
- ENGERIX-B®
- RECOMBIVAX HB®
- HEPLISAV-B™
Combination vaccines
- PEDIARIX®: Combined hepatitis B, diphtheria, tetanus, acellular pertussis (DTaP), and inactivated poliovirus (IPV) vaccine. Cannot be administered before age 6 weeks or after age 7 years.
TWINRIX®: Combined Hepatitis A and hepatitis B vaccine. Recommended for people aged ≥18 years who are at increased risk for both HAV and HBV infections.
What are the recommended schedules for hepatitis B vaccination?
The vaccination schedule most often used for children and adults is three intramuscular injections, the second and third doses administered at 1 and 6 months, respectively, after the first dose. Alternate schedules have been approved for certain vaccines and/or populations. A new formulation, Heplisav-B (HepB-CpG, manufactured by Dynavax), is approved for two doses, 1 month apart.
What are the recommended doses of hepatitis B vaccines?
| Age Group | Single-antigen vaccine | Combination vaccine | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Recombivax HB | Engerix-B | Heplisav-B | Pediarix † | Twinrix § | |||||||
| Dose (μg) ¶ | Vol(mL) | Dose (μg) ¶ | Vol(mL) | Dose (μg) ¶ | Vol(mL) | Dose (μg) ¶ | Vol (mL) | Dose (μg) ¶ | Vol (mL) | ||
| Infants (<1 yr) | 5 | 0.5 | 10 | 0.5 | – | – | 10† | 0.5 | NA** | NA | |
| Children (1–10 yrs) | 5 | 0.5 | 10 | 0.5 | – | – | 10† | 0.5 | NA | NA | |
| Adolescents | 11–15 yrs | 10†† | 1.0 | NA | NA | – | – | NA | NA | NA | NA |
| 11–19 yrs | 5 | 0.5 | 10 | 0.5 | – | – | NA | NA | NA | NA | |
| Adults (≥18 yrs) | – | – | – | – | 20 | 0.5 | – | – | 20§ | 1 | |
| Adults (≥20 yrs) | 10 | 1 | 20 | 1 | 20 | 0.5 | NA | NA | 20§ | 1 | |
| Hemodialysis patients | <20 yrs §§ | 5 | 0.5 | 10 | 0.5 | 20 | 0.5 | NA | NA | NA | NA |
| ≥20 yrs | 40¶¶ | 1 | 40*** | 2.0 | 20 | 0.5 | NA | NA | NA | NA | |
† Combined hepatitis B, diphtheria, tetanus, acellular pertussis adsorbed, inactivated poliovirus vaccine. This vaccine cannot be administered at birth, before age 6 weeks, or at age ≥7 years.
§ Combined Hepatitis A and hepatitis B vaccine. This vaccine is recommended for people aged ≥18 years who are at increased risk for both hepatitis B virus and Hepatitis A virus infections.
¶ Recombinant hepatitis B surface antigen protein dose.
** Not applicable.
†† Adult formulation administered on a 2-dose schedule.
§§ Higher doses might be more immunogenic, but no specific recommendations have been made.
¶¶ Dialysis formulation administered on a 3-dose schedule at 0, 1, and 6 months.
*** Two 1.0-mL doses administered at one site, on a 4-dose schedule at 0, 1, 2, and 6 months.
Who should not receive hepatitis B vaccine?
Anyone who has had a serious allergic reaction to a prior dose of hepatitis B vaccine, a component of the hepatitis B vaccine, or yeast should not receive hepatitis B vaccine. When hepatitis B vaccine is administered as part of a combination vaccine, contraindications to other vaccines should be checked.
Can a patient receive the first dose of hepatitis B vaccine from one manufacturer and subsequent doses from another manufacturer?
Yes. When feasible, vaccines from the same manufacturer should be used to complete the series, but vaccination should not be deferred when the manufacturer of the previously administered vaccine is unknown or when the vaccine from the same manufacturer is unavailable. Different vaccination schedules apply for patients receiving vaccines from different manufacturers; details regarding how to complete the vaccination series using vaccine from a different manufacturer are available. Data are limited on safety and immunogenicity when HepB-CpG is interchanged with HepB vaccines from other manufacturers (15).
If there is an interruption between doses of hepatitis B vaccine, does the vaccine series need to be restarted?
No. The series does not need to be restarted, but the following should be considered.
- If the vaccine series was interrupted after the first dose, the second dose should be administered as soon as possible.
- The second and third doses should be separated by an interval of at least 8 weeks.
- If only the third dose is delayed, it should be administered as soon as possible.
Is it harmful to administer an extra dose(s) of hepatitis B vaccine or repeat the entire vaccine series if documentation of vaccination history is unavailable?
No. If necessary, administering extra doses of single-antigen hepatitis B vaccine is not harmful.
Can hepatitis B vaccine be administered concurrently with other vaccines?
Yes. Administering hepatitis B vaccine at the same time as other vaccines has not been shown to interfere with antibody response. Separate body sites and syringes should be used for simultaneous administration of injectable vaccines.
How long does protection from hepatitis B vaccine last?
Studies indicate that immunologic memory remains intact for at least 30 years among healthy people who initiated hepatitis B vaccination at >6 months of age (16). The vaccine confers long-term protection against clinical illness and chronic hepatitis B virus infection. Cellular immunity appears to persist even though antibody levels might become low or decline below detectable levels (17). Among vaccinated cohorts who initiated hepatitis B vaccination at birth, long-term follow-up studies are ongoing to determine the duration of vaccine-induced immunity (16).
Why should an infant receive hepatitis B vaccine at birth before hospital discharge, even if the mother is negative for hepatitis B surface antigen (HBsAg)?
ACIP recommends that all infants receive hepatitis B vaccine at birth, regardless of the infection status of the mother (15). Infants born to HBV-infected mothers require hepatitis B vaccine and hepatitis B immune globulin (HBIG) within 12 hours of birth to protect them from infection. However, because errors or delays in testing, reporting, and documenting maternal HBsAg status can and do occur, administering the first dose of hepatitis B vaccine soon after birth to all infants acts as a safety net, reducing the risk for perinatal infection when maternal HBsAg status is either unknown or incorrectly documented at delivery. Also, initiating the hepatitis B vaccine series at birth has been shown to increase a child's likelihood of completing the vaccine series on schedule (15)
Should pregnant women be tested for HBV?
Yes. Women should receive HBsAg testing during each pregnancy, and those who are HBsAg-positive should have HBV DNA testing. AASLD recommendsexternal icon that HBsAg-positive pregnant women with HBV DNA levels of >200,000 IU/ML be provided antiviral therapy to reduce perinatal HBV transmission (18).
Can hepatitis B vaccine be given during pregnancy or lactation?
Yes. The hepatitis B vaccine contains no live virus, so neither pregnancy nor lactation should be considered a contraindication to vaccination. Of the three available adult vaccines for hepatitis B, there is limited safety data for HEPLISAV-B, and as such, providers should continue to vaccinate pregnant women needing hepatitis B vaccination with a vaccine from a different manufacturer. Limited experience suggests that the developing fetus is at no apparent risk for adverse effects when hepatitis B vaccine is administered to pregnant women (19). Meanwhile, new HBV infection in a pregnant woman might result in severe disease for the mother and chronic infection for the newborn. Pregnant women who are identified as being at risk for HBV infection during pregnancy should be vaccinated and counseled concerning other methods to prevent HBV infection. Pregnant women may be at increased risk for hepatitis B if they
- have had more than one sex partner during the previous 6 months,
- are being evaluated or treated for a sexually transmitted infection,
- have had recent or current injection-drug use, or
- have had a HBsAg-positive sex partner.
Can pregnant women get the HEPLISAV-B vaccine?
There are no published clinical studies of HEPLISAV-B in pregnant women. Available human data on HEPLISAV-B administered to pregnant women are insufficient to inform assessment of vaccine-associated risks in pregnancy. Until safety data are available for HEPLISAV-B, providers should continue to vaccinate pregnant women needing hepatitis B vaccination with a vaccine from a different manufacturer.
Providers and patients can report administration of HEPLISAV-B to a pregnant woman to the HEPLISAV-B® Pregnancy Registry, an observational study being conducted in the United States to evaluate pregnancy outcomes in women vaccinated with HEPLISAV-B® within 28 days prior to conception or at any time during pregnancy. The Registry is sponsored by Dynavax Technologies Corporation and is managed by Pharmaceutical Product Development (PPD), Inc.
- Toll-free number: 1-844-443-7734
- Email: heplisavbpregnancyregistry@ppdi.com
A pregnancy exposure registryexternal icon is a study that collects health information from women who take prescription medicines or vaccines when they are pregnant.
Can hepatitis B vaccine be given to immunocompromised people, such as people on hemodialysis or people with HIV?
Yes. A larger vaccine dose is required to induce protective antibody in hemodialysis patients, and larger or additional doses might also be necessary for other immunocompromised people. Serologic testing of hemodialysis patients and other immunocompromised people is recommended 1–2 months after administration of the final dose of the primary vaccine series to determine the need for revaccination. Detailed guidance on vaccination of hemodialysis patients and other immunocompromised people is available from the Advisory Committee on Immunization Practices recommendations on adult hepatitis B vaccination pdf icon [40 pages].
Can hepatitis B vaccine be given after exposure to HBV?
Yes. After a person has been exposed to HBV, appropriate prophylaxis, given as soon as possible but preferably within 24 hours, can effectively prevent infection. The mainstay of postexposure immunoprophylaxis is hepatitis B vaccine, but, in certain circumstances, the addition of HBIG provides increased protection (20,21).
Should people be tested for immunity to hepatitis B before being vaccinated?
Adult populations with risk factors for HBV transmission or at risk for HBV reactivation should receive complete serologic testing (HBsAg, anti-HBs, and anti-HBc) so they can be appropriately counseled, vaccinated, and/or linked to care and treatment. (See Who should be screened for HBV? for information about who should receive pre-vaccination testing.)
The first vaccine dose should be administered immediately after collection of the blood sample for serologic testing. Vaccinating people who are immune to HBV infection because of current or previous infection or vaccination is not harmful and does not increase the risk for adverse events.
For people determined to be HBsAg negative, no further action is required. People with positive HBsAg should be referred to a specialist in the management of hepatitis B infection and receive further serologic evaluation, prevention counseling, and evaluation for antiviral treatment (see Management of HBsAg-Positive Persons). People who are anti-HBc positive should be counseled about their prior exposure to HBV and potential risk for HBV reactivation.
Is there any benefit in or risk associated with vaccinating a person who has been infected with HBV?
No. People who have already been infected with HBV will receive no benefit from vaccination. Vaccinating someone who is already infected poses no risk to the patient.
Who should receive postvaccination testing?
Testing for immunity is advised only for people whose subsequent clinical management depends on knowledge of their immune status, including
- infants born to HBsAg-positive mothers; https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6439a6.htm
- health-care workers and public safety workers at high risk for continued percutaneous or mucosal exposure to blood or body fluids; https://www.cdc.gov/mmwr/preview/mmwrhtml/rr6210a1.htm
- chronic hemodialysis patients, people with HIV, other immunocompromised people (e.g., hematopoietic stem-cell transplant recipients or people receiving chemotherapy); and
- sex partners of people with chronic HBV infection.
When should postvaccination testing be done in infants born to HBsAg-positive mothers?
For infants born to HBsAg-positive mothers, postvaccination testing should be performed 1–2 months after completion of ≥3 doses of a licensed hepatitis B vaccine series. Testing should not be performed before age 9 months in order to avoid detection of anti-HBs from hepatitis B immune globulin (HBIG) administered during infancy and to avoid detection of HBsAg from vaccine (HBsAg can be transiently positive for 1–18 days after vaccination). Testing at 9 months or later also maximizes detection of late HBV infection. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6439a6.htm
Can anti-HBs levels following vaccination decline over time?
Yes. Following vaccination, anti-HBs levels decline over time. Anti-HBs ≥10 mIU/mL is considered a correlate of vaccine-induced protection for people who have completed an approved vaccination series. Immunocompetent people who achieve an anti-HBs level ≥10 mIU/mL 1–2 months after completing the hepatitis B vaccine series remain protected, even if anti-HBs levels decline to <10 mIU/mL beyond that time (presumably because of persistent cellular immunity). https://www.cdc.gov/mmwr/preview/mmwrhtml/rr6210a1.htm
Are booster doses of hepatitis B vaccine recommended?
Booster doses are not recommended for people with normal immune status who have been vaccinated (16,22). Only certain people should receive a booster dose in specific situations. For hemodialysis patients, if annual testing for antibody to hepatitis B surface antigen (anti-HBs) shows a decline to <10 mlU/mL, a booster dose should be administered. For other immunocompromised people (including those with HIV, hematopoietic stem-cell transplant recipients, and people receiving chemotherapy), the need for booster doses has not been determined. When anti-HBs levels decline to <10 mIU/mL, annual anti-HBs testing and booster doses should be considered for those with an ongoing risk for exposure.
References
1. Centers for Disease Control and Prevention. Viral hepatitis surveillance—United States, 2017. Atlanta: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2019. Available at: https://www.cdc.gov/hepatitis/statistics/2017surveillance/index.htm.
2. Bond WW, Favero MS, Petersen NJ, Gravelle CR, Ebert JW, Maynard JE. Survival of hepatitis B virus after drying and storage for one week. Lancet. 1981;1(8219):550–1.
3. LeFevre ML. Screening for hepatitis B virus infection in nonpregnant adolescents and adults: US Preventive Services Task Force recommendation statement. Annals Internal Med. 2014;161(1):58–66.
4. Lok AS, McMahon BJ. AASLD practice guideline update. Hepatology. 2009.
5. Weinbaum CM, Mast EE, Wang SA, et al. Recommendations for identification and public health management of persons with chronic hepatitis B virus infection. Morbidity and Mortality Weekly Report 2008;19(57 [No. RR–8]):1–20.
6. Fattovich G, Bortolotti F, Donato F. Natural history of chronic hepatitis B: special emphasis on disease progression and prognostic factors. J Hepatol. 2008;48(2):335–52.
7. Hoofnagle JH, Di Bisceglie AM. Serologic diagnosis of acute and chronic viral hepatitis. Semin Liver Dis. 1991;11(2):73–83.
8. Krugman S, Overby LR, Mushahwar IK, Ling CM, Frosner GG, Deinhardt F. Viral hepatitis, type B. Studies on natural history and prevention re-examined. N Engl J Med. 1979;300(3):101–6.
9. Beasley RP. Hepatitis B virus. The major etiology of hepatocellular carcinoma. Cancer. 1988;61(10):1942–56.
10. McMahon BJ. The natural history of chronic hepatitis B virus infection. Hepatology. 2009;49(5 Suppl):S45–55.
11. Abara WE, Qaseem A, Schillie S, et al. Hepatitis B vaccination, screening, and linkage to care: best practice advice from the American College of Physicians and the Centers for Disease Control and Prevention. Ann Intern Med. 2017;167(11):794–804.
12. Terrault NA, Bzowej NH, Chang KM, Hwang JP, Jonas MM, Murad MH. AASLD guidelines for treatment of chronic hepatitis B. Hepatology. 2016;63(1):261–83.
13. Hsu C, Tsou HH, Lin SJ, et al. Chemotherapy-induced hepatitis B reactivation in lymphoma patients with resolved HBV infection: a prospective study. Hepatology. 2014;59(6):2092–100.
14. Mücke MM, Backus LI, Mücke VT, et al. Hepatitis B virus reactivation during direct-acting antiviral therapy for hepatitis C: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2018 Mar;3(3):172–180.
15. Schillie S, Harris A, Link-Gelles R, Romero J, Ward J, Nelson N. Recommendations of the Advisory Committee on Immunization Practices for use of a hepatitis B vaccine with a novel adjuvant. MMWR Morb Mortal Wkly Rep 2018;67:455–8.
16. Bruce MG, Bruden D, Hurlburt D, et al. Antibody levels and protection after hepatitis B vaccine: results of a 30-year follow-up study and response to a booster dose. J Infect Dis. 2016;214(1):16–22.
17. Middleman AB, Baker CJ, Kozinetz CA, et al. Duration of protection after infant hepatitis B vaccination series. Pediatrics 2014;133(6).
18. Pan CQ, Duan Z, Dai E, et al. Tenofovir to prevent hepatitis B transmission in mothers with high viral load. N Engl J Med. 2016;374(24):2324–34.19. Schillie S, Vellozzi C, Reingold A, et al. Prevention of Hepatitis B Virus Infection in the United States: Recommendations of the Advisory Committee on Immunization Practices. MMWR Recomm Rep. 2018; 67(1);1–31.
20. Schillie S, Murphy TV, Sawyer M, et al. CDC guidance for evaluating health-care personnel for hepatitis B virus protection and for administering postexposure management. MMWR Recomm Rep. 2013;62(RR–10):1–19.
21. CDC. Updated U.S. Public Health Service guidelines for the management of occupational exposures to HBV, HCV, and HIV and recommendations for postexposure prophylaxis. MMWR Recomm Rep. 2001;50(RR–11):1–52.
22. Leuridan E, Van Damme P. Hepatitis B and the need for a booster dose. Clin Infect Dis. 2011;53(1):68–75.
7.1 Finding Rational Solutions of Polynomial Equations a B Answers
Source: https://www.cdc.gov/hepatitis/hbv/HBVfaq.htm